Purpose
Phase 1 of the Fit2Sit pilot provided Paramedics with specific criteria to identify
low-acuity patients that could be safely offloaded to the ED waiting room following a
full triage report.
Phase 2 of the Fit2Sit program is designed to determine whether certain, low-acuity patients can be offloaded to the ED waiting room to safely self-triage prior to the traditional “complete” hospital triage process. Phase 2 aims to:
- Improve hospital transfer of care (HTOC) performance, and
- Reduce Paramedic in-hospital time.
It is anticipated that hospitals will also experience an improvement (decrease) in triage wait times for higher priority patients, as well as reduced congestion in the ED.
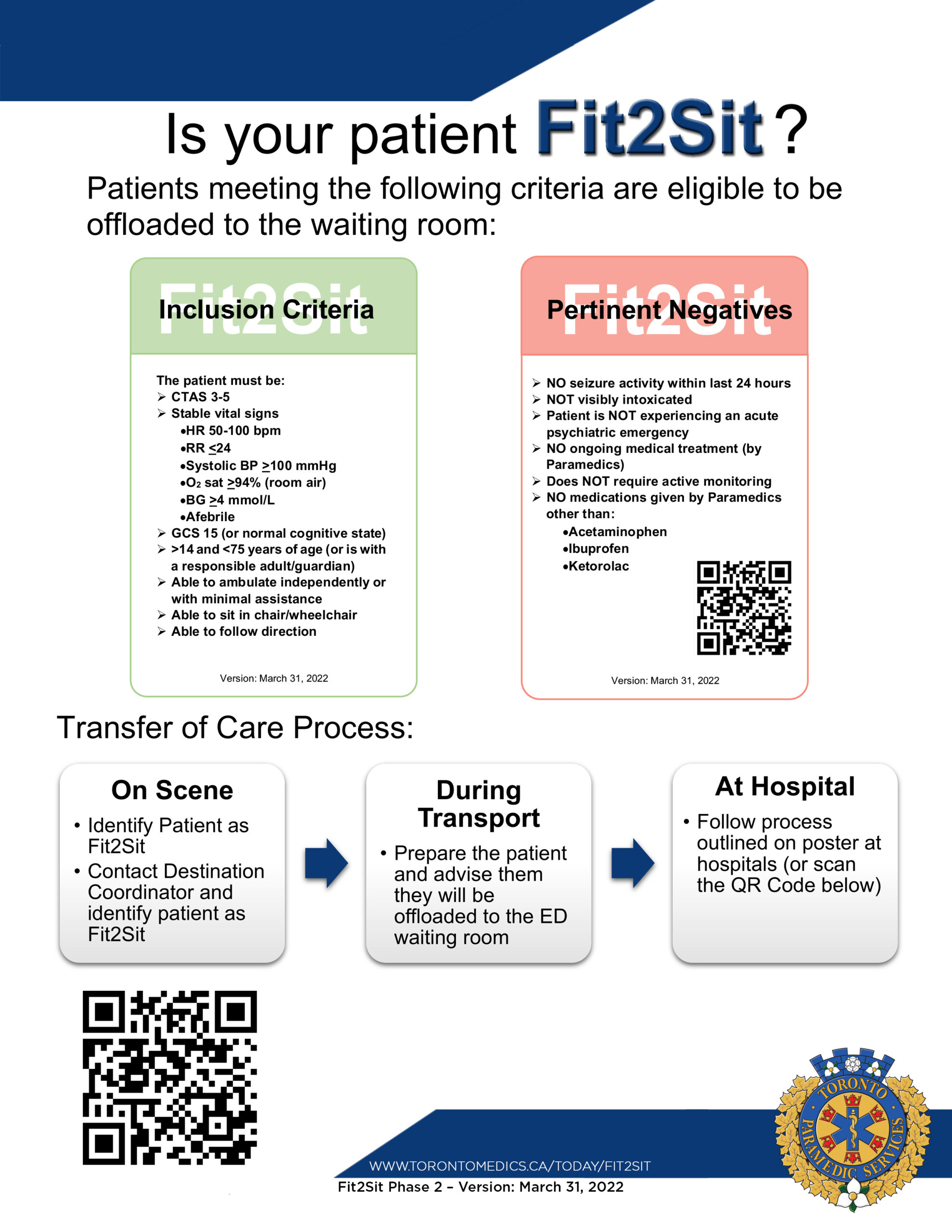
- Patients are deemed appropriate for the Fit2Sit program by Paramedics while on scene (i.e., all inclusion and exclusion criteria have been met). Paramedics are expected to explain the receiving hospital’s process to the patient/escort.
- The Toronto Paramedic Services (TPS) Communications Centre will be notified that the patient meets Fit2Sit criteria when Paramedics request a hospital destination. This will prompt a specific selection/entry in the Patient Destination Software (PDS). The patient will then be assigned to a receiving hospital and transported there by ambulance.
- PDS will indicate incoming Fit2Sit patients with a symbol in the special distribution column of the ‘En-Route EMS Units’ queue.
- Paramedics are expected to prepare the patient for the Fit2Sit transfer of care process during transport. A set of vital signs should be taken close to hospital arrival to confirm Fit2Sit criteria are still met. The vital signs and time taken are to be recorded on the Fit2Sit Paramedic Report (see Appendix 2) in addition to the ePCR.
- Upon arrival at the ED, Paramedics will bring the patient into the hospital via the agreed upon entrance. The hospital process (see Appendix 5) for each site can be found by scanning the QR code on the Fit2Sit Paramedic Reference card (see Appendix 1) and the Fit2Sit Ambulance Poster (see Appendix 4).
- Paramedics will immediately offload the patient to the designated Fit2Sit area provided by the hospital using either a chair or wheelchair, as appropriate.
- Paramedics will wait for the next available triage nurse and provide:
- A brief verbal report; and
- The signed and completed Fit2Sit Paramedic Report. Paramedics will note the current time (i.e., the time the verbal report is given) on the Fit2Sit Paramedic Report.
- Hospital Transfer of Care (HTOC) is deemed to have occurred when the triage nurse has received both the verbal report and Fit2Sit Paramedic Report. The triage nurse (or designate) will update the status of the applicable TPS vehicle in PDS to confirm and display HTOC.
- Paramedics will contact the TPS Communications Centre (e.g., Hospital Clearing Coordinator) and update their status to Paramedic Transfer of Care (PTOC) following the completion of step 7.
- The patient will remain in the designated waiting area and will self-triage according to hospital process.
- The patient will maintain care of their health card, personal belongings, and medications.
- The triage nurse (or designate) will ensure that the Fit2Sit Paramedic Report is included in the patient’s hospital file.
- Paramedics will complete their ePCR in accordance with TPS policy.
In compliance with current MOH Basic Life Support Patient Care Standards and Advanced Life Support Patient Care Standards, all required information will be provided to the hospital in the format set out below.
Verbal Report
The Paramedic will provide a brief verbal report to the triage nurse that must include:
- Confirmation of the patient’s status as a Fit2Sit candidate;
- The patient’s Infectious Disease Screening status (according to current standards and practice);
- Patient name, age, sex and CTAS level (Arrive Destination);
- Patient’s Chief complaint;
- A concise history of the patient’s current problem(s) and relevant past medical history;
- Pertinent assessment findings and vital signs; and
- Pertinent management performed and responses to management.
Note: Paramedics may report “stable vital signs” in place of verbally stating each vital sign. Actual numerical values on of the patient’s vital sign are reported on the Fit2Sit Paramedic Report. Patients must be vitally stable in order to qualify as Fit2Sit.
The Fit2Sit Paramedic Report is to be completed by the Paramedic prior to reporting to the triage nurse. The Paramedic will record the verbal triage report time on the Fit2Sit Paramedic Report.
The Fit2Sit Paramedic Report includes:
- Date of Report
- Patient Name
- Patient Date of Birth (DOB)
- Patient Chief Complaint
- Vehicle Number
- Run Number
- Trip Number
- Arrived Hospital Time
- One complete set of vital signs (or two sets of vital signs if approved medication was given). Recorded vital signs should be taken close to hospital arrival to confirm Fit2Sit criteria are still met and include:
- Time
- Blood pressure
- Heart rate
- Respiratory rate
- Temperature
- Oxygen saturation
- Blood glucometry (if indicated)
- Signature of Paramedic confirming that the patient met all criteria for Fit2Sit at time of transfer of care
- Time of verbal report
The Paramedic will document a complete set of vital signs on the Fit2Sit Paramedic Report as detailed above:
- If medications were NOT administered, the most recent set of vital signs will be recorded on the report (previous vital signs will be captured on the ePCR).
- If medications were administered to the patient, two sets of vital signs must be recorded on the report. The most recent set of vital signs (i.e. obtained prior to HTOC) must be recorded at least 15 minutes post-treatment.
The Paramedic will tear off the bottom portion of the Fit2Sit Paramedic Report (with the tracking number) and enter the tracking number in the appropriate section of the ePCR.
The Paramedic will sign and record the transfer of care (HTOC) time on the Fit2Sit Paramedic Report following the verbal report, and deliver the Fit2Sit Paramedic Report to the triage nurse.
Following HTOC, the triage nurse will obtain any additional information directly from the patient, consistent with the hospital’s regular triage process. Paramedics are not required to remain with the patient or provide further reports following HTOC.
Fit2Sit has been added to the ‘General Admin’ section of the ePCR application. There are three sections that Paramedics will need to complete:
- Pt Fit2Sit?
- Paramedics will be required to choose 1 of three options
- Patient meets Fit2Sit criteria/enrolled;
- Patient meets Fit2Sit criteria/not enrolled; or
- Patient does not meet Fit2Sit criteria.
- If not enrolled Fit2Sit. Reason?
- Paramedics are to provide a reason for not enrolling their patient as Fit2Sit when they met the criteria.
- For patients that were enrolled or did not meet the Fit2Sit criteria, Paramedics should write N/A.
- Fit2Sit Tracking number.
- The Fit2Sit tracking number is required to be entered for all patients enrolled in Fit2Sit. This can be found on the portion of the Fit2Sit Paramedic Report that should have been torn off prior to handing the form over to triage (or designate).
NOTE: The Fit2Sit questions in the ePCR must be completed in order for the call to be closed and marked as complete (i.e., a ‘closed call rule’).
A Fit2Sit QA program is in place with oversight by TPS Professional Standards Unit to ensure all aspects of the program are regularly reviewed. TPS will perform manual compliance audits on the first 500 qualifying patients subject to the program (combined from all participating hospitals). All documentation on qualifying patients will undergo a binary audit. Manual audits will be performed as required and as outlined in the Fit2Sit QA program.
The Fit2Sit Hospital Feedback Form (see Appendix 3) is to be completed by hospital staff for all:
- Fit2Sit patients where hospital staff (e.g., triage nurse) believe the patient did not meet Fit2Sit criteria at the time of triage; and/or
- Fit2Sit patients that deteriorate within the first 60 minutes following HTOC.
The Fit2Sit Feedback Forms will be reviewed by TPS in a timely manner and results of the review will be shared with the submitting hospital.





Below is an example of the posters that will display the hospital flow process for each site. Final Hospital Process Flow Charts will be released with the “Go Live” memo and will be accessible through the QR code.

