Since Fit2Sit was implemented one year ago, Paramedics have enrolled more than 4000 patients, and the continuous quality assurance review has demonstrated the program’s safety when the inclusion and exclusion criteria are followed.
Based on feedback from Paramedics and with support from our hospital partners, qualifying Fit2Sit patients will now have greater flexibility in their hospital destination choice.
The Hospital Destination Coordinator (HDC) will follow the current process for destinating a Fit2Sit patient; however, effective December 21, 2023, PDS will now provide up to three hospital options.
The HDC shall provide the Paramedic crew with the first hospital option displayed in PDS. If the Paramedic requests a specific hospital and it is one of the three options displayed, the HDC may select this hospital destination.
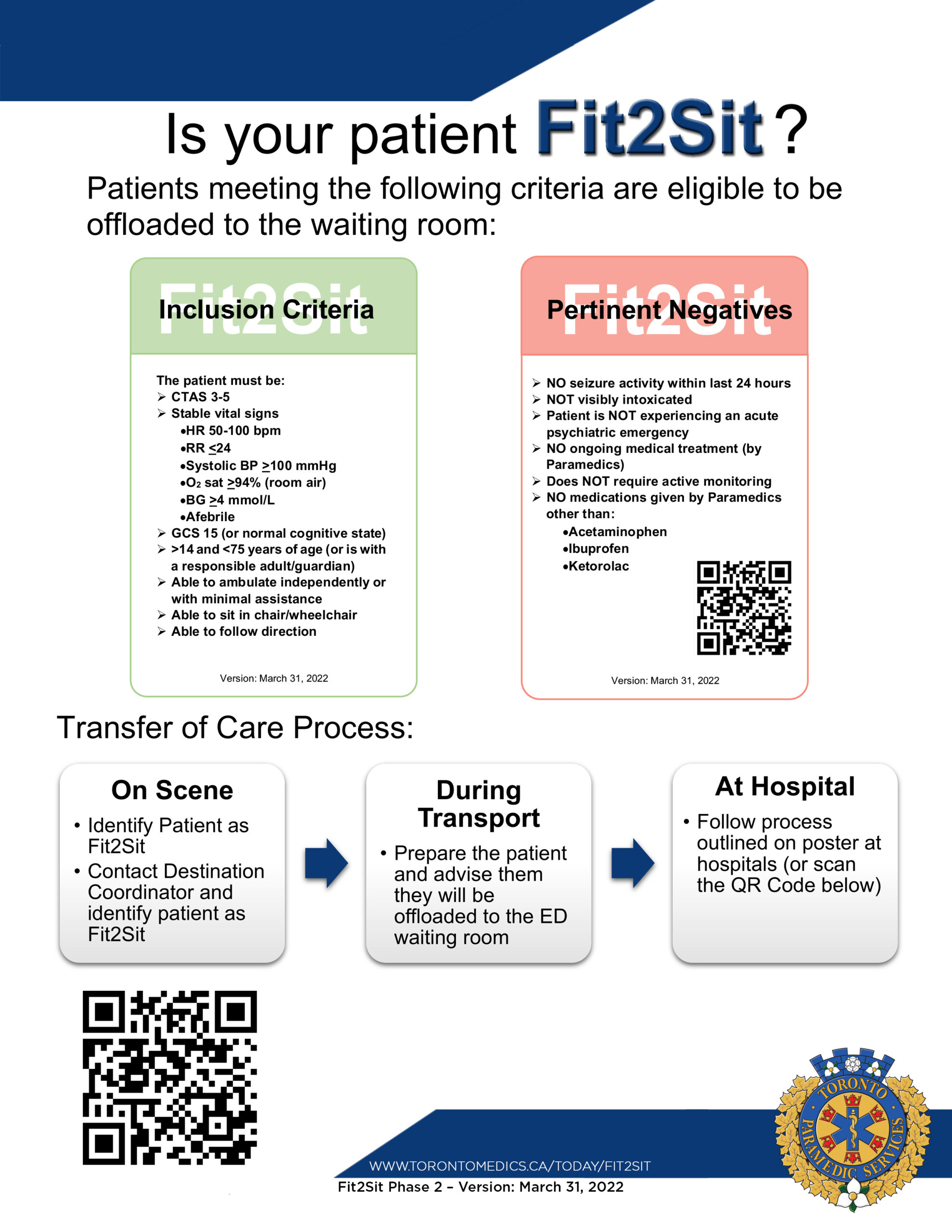
Additional PDS Fit2Sit criteria:
- If the transport time to a hospital is greater than 16 minutes, it will be automatically excluded from the PDS hospital recommendations.
- Fit2Sit will only be allowed by PDS for patients who are CTAS 3-5.
- PDS will assign 15 minutes of ‘Time to Next Patient’ (TNP) credit for all Fit2Sit Patients.
Paramedics may use the term “ambulatory” when requesting a hospital destination. However, this term has no impact on the hospital options shown by PDS and there is no action for the HDC to take when it is included in the destination request. As a reminder, the ‘Fit2Sit’ option in PDS is for Fit2Sit patients only and should not be used for an ambulatory patient. Offloading the Fit2Sit patient to the waiting room is at the discretion of the Paramedic and not the hospital.
If you have any questions or concerns, please speak to your Superintendent.
Sincerely,
(Original signed by)
Jennifer Chung







You must be logged in to post a comment.